“Why do you do that to yourself?”
Why would I not? That’s the more pointed question.
I remember being lazy. I was fit, well, and always a little dissatisfied. …This might be the human condition.
I loved to work (still do) but I also valued my downtime, time in the wild, beach time, workout time, hang time with friends. Something like work-life balance, I guess. In retrospect it seems lazy, but my perspective is a little distorted. It’s been decades since I had a real vacation from my current work.
Current work situation
My current work is living anyway, in spite of this suite of deficits and dysfunctions. It doesn’t give me time off. It’s frankly a bit tiresome.
Why, yes, that was a supremely wry understatement. Cackle freely!
If I stuck to doing only the things that hurt the least, stress my system the least, and otherwise rock this boat as little as possible, what would happen?
Would I be more comfortable? Actually… no, not beyond the time that rest is necessary and productive.
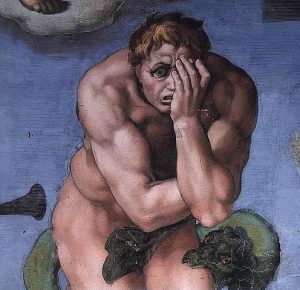
Would I get any better? Decidedly not. “Use it or lose it” beats in my mind like a metronome when I’m down too long. If I don’t stay active, right up to current limits, my exertional malaise gets worse. (It’s a real thing: exercise tears the body down, where it would build a normal person’s up.)
Survival of the fittest
“Then, let’s be honest here, do you deserve to survive?”
Most (not all) people ask that more subtly, but it’s a question I’ve faced often. Brutal it may be, but it’s natural.
First, let’s check the wording. The phrase “survival of the fittest” was coined by the economic theorist & philospher Herbert Spencer (who clearly didn’t let clarity stand in the way of a good bumper-sticker slogan.)
Darwin later adopted it, possibly assuming that his accompanying thoughts would be kept in mind. Now we have to specify them: strength, speed, intelligence, etc., are all subordinate to being able and willing to adapt to change.
The point he was making all along is that they key to survival is adapting to change. Not being in shape.
Finches aren’t humans
Darwin famously studied tiny birds on tiny islands to arrive at his insights. They had tiny life spans and tiny jobs. For them, fitness was biological: who got to breed and have their offspring get to breed, and so on ad infinitum? Breeding and brooding are simple markers.
Humans have big, tangled societies with big, tangled networks and big, tangled obligations. It’s not just breeding and brooding, although that can be part of it. It’s work, school, friends, parents, neighbors, politics & policy, insurance premiums, mutual aid, prepping for a blizzard or another record-breaking hurricane. This time of epochal shifts in weather, science, and economics creates a relentless roar of things we need to cope with and adapt to, and a life where breeding & brooding cannot ensure survival, because, for many, the money and assurance of a tolerable future just aren’t there any more. Only appropriate adaptation to change can aid survival.
We’re (almost) all forced to manage so much more than the finches ever could conceive of.
Stating the obvious
What group of people is the best at adapting?
Take a minute. I’m not going anywhere.

Who else but your people with handicaps and disabilities.
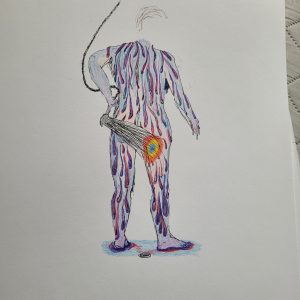
Watch what they do, how they manage in the face of an intransigent world and variable limits, how they keep going. It looks like an art form, if life itself were art.
Just the cost of doing business
I’m still absorbing an incident ~12 years ago when a chair-riding friend with paraplegia was driving us in his van, and we had to stop and get gas. I unbuckled my seatbelt and was going to go pump. He waved me down. “Nah, I got it.”
He opened the sliding door behind him, flicked his wheelchair out of the minivan and half-open in one complicated motion, levered himself and the chair into conjunction, and went on about the business of pumping gas from his chair. Then he reversed the process (more or less) to get back in.
I told him that was impressive. Didn’t he mind the effort?
He shrugged. “It’s just the cost of doing business.”
I let that sink in.
Everybody has to do tedious things to get to the next thing they want. It’s the cost of doing business, of getting through life.
Everybody’s cost is a bit different.
Everybody should have the right to choose what’s worth the cost.
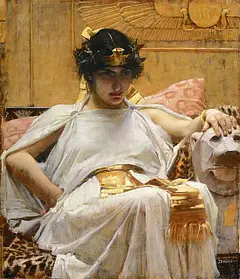
“Life, liberty, and the pursuit of happiness” was originally written in bloody-handed hypocrisy, but it’s right and wise to make it true.
Challenging yourself can be fun
With all that said, my insistence on pushing my limits — as long as I can generally expect safe air, food, water, shelter, and adequate rest — might make more sense. Or maybe it doesn’t. It’s not likely to change, especially since I decided last year that life was too short to settle for survival — I was going to chase fun, and see where I found it!