[Follow this link for the audio version: https://www.spreaker.com/episode/2024-09-07-1staidatroadside–61297573]
I headed to psychotherapy after texting, “I’m on my way. I’ll see you in person today, barring the unexpected”
I was feeling a bit cautious, because a couple hours before, the thought had come to me, “when things get hectic, trust your training.”
What training? Was I about to have a series of intrusive thoughts harking back to the times I’ve had to file restraining orders, one of which magically disappeared and I had to flee the area – right before Christmas? I hoped not. Martial arts training has certainly come in handy, but come on…
No, no intrusive thoughts, but I did wonder which set of training I should have in mind.
A few miles down the interstate, I saw a pickup truck stopped dead, and a sedan facing it.
People were only just getting out of the truck. I put my flashers on and pulled in behind.
I definitely trust my training in this kind of situation. I put my anxiety to one side and sailed in.
The only person to worry about was a littlie in the back of the sedan. Had spontaneous pulse – a good one – and respirations. He could speak, to the limit of saying, “I want my Mommy” (sound of heart-strings tearing), so I checked his spine at his neck. It was there, but not quite right. Once he could speak more, he told me his neck hurt where I touched it (I’d been holding his head & neck stable since I felt it). As I told the fire department medic later, “on me, it’d be a chiropractic adjustment. On a littlie that age, I’m not sure.” He nodded and sent his buddy in with a pediatric cervical collar.
Littlie’s mother was on the phone the whole time with him. So much love swirling around in that car. I told the Dad that I noticed it, and that it’s healing.
At each stage – or rather, just before the next round of excitement – I explained to Littlie that there would be more people, highly trained people who really cared about him being okay. Let him know roughly what to expect at each stage. Coached him to go along with things as well as he could. When the fireman asked him to squeeze his finger, he squeezed my hand instead (sound of heart melting).
I could see most of my words going over his head (as expected), but I could also see the sense of reason and structure calming his exhausted and shocky brain so he could tune in a little more.
I grew up in a musical household, so naturally I hummed pretty little made-up tunes and it visibly calmed him – and possibly his parents too, a little.
I’ve been working on learning how to stabilize a shocky system for 25 years, on top of my trauma nursing work. I’m only a patient – and a nerd – but still, I have lots of good training. I trusted my training in that, too.
I gave his mother my number right before the fire department and EMTs rolled up. I think it was a training day, because there were 7 or 8 more people there, one of them a cheerful charming know-it-all (every team needs one of those) who got the best responses out of Littlie.
I let the kid know I had to go but his Mommy would stay on the phone with him and he’d be cared for by these really nice people. Told his Mom I loved her kid and he was terrific (sound of heart-strings pulling).
Once his c-collar was on (definitely a training day; I helped get it positioned and sealed correctly in the end) and they had the gurney ready, I realized I had to stand up. After perching my crippled butt by one hip on a steel door frame for half an hour. In front of people. Specifically, a total of 9 or 10 fit, athletic slabs of beef (-cake) no less than 10 years younger than me, and most of them half my age.
This was not going to be great for the ego, but I knew I could get a laugh out of it.
So I used both arms and every available leg (which was slightly less than 2) to lever myself upward, saying, “I’m an *oooold* trauma nurse” by way of cover, and squirmed through the kindly, protective testosteronic press and into fresh air.
I signed off with everybody and retreated to my comfy car.
I called my psychotherapist and said, “Remember what I said about ‘barring the unexpected?’…”
We had a phone session once I was safely off on a side street and in a proper parking space. She was full of commentary about how I applied those psych skills and met psychosocial and informational needs appropriately, as well as the nursey stuff. So yeah, that was good…
… because my brain was churning constantly about every single moment and thought and decision for an entire hour. Looking for a fault. Looking for something I’d missed or where my training had lapsed or been forgotten. Cycling through, over and over, looking for any lapse.
This used to be how I improved my skills – look for errors, even tiny ones, and figure out how to prevent or avoid them in future. Now, it’s just my ADHD brain torturing me.
And computer says Nope. Failed to suck. I’m pretty sure I failed to suck. That’s a relief.
I’ve been thinking about it pretty much nonstop, but rather than worrying myself woolly, I got an organizing thing for my car and picked up some food. Both of these are calming, grounding things, perfect for pulling my adrenaline out of the stratosphere.
Then I crawled home and had fresh corn and gluten-free carrot cake for dinner. It’s good to have a little sweetness when your body is still convinced the world is full of excoriation.
I’ve had no calls from them and I don’t expect one. They’ve got to be absolutely wrung out regardless of how things went. The kid comes first, and then comes their own care and self-management.
They don’t have to think of me ever again: I know how shocking and painful it could be to revisit the moment.
I’d love to know. I hope like crazy that the kid came out of it OK. I never got to follow up with patients when I was a nurse (because confidentiality), and I’d sure appreciate it if this family wanted to give me a heads-up just to soothe that old itch.
All that being said, I want all you non-nurses to know that they don’t owe me one word of contact or one moment of concern. I was in the right place at the right time with the right training, and I trusted my training. That’s what we do.
They have the hard part: figuring out next steps with a shook-up and possibly injured Littlie who was going home early because he was already ill.
That kid was having a rotten day.
I sure hope it got better.
Forestalling future problems
I don’t have a jump-kit for my car. That could be a problem in the future. I was lucky this time because all I needed was my brain, arms, hands, and voice.
It’s probably the 6th or 7th accident I’ve stopped at and I really do know what’s needed at the roadside – and it isn’t much. I used to get confused by the fact that I didn’t have a stethoscope, oxygen on tap, i.v. gear, and All Tha Meds. Once I’m on scene, though, it gets very easy.
Any blood or, indeed, anything wet? Nitrile gloves, packed up in pairs and stowed in a closed outer pocket to keep them clean & dry and easy to get on.

Heaven forbid, does anybody need CPR? This very rarely happens, but when it does, I don’t want to have to dig for the needful. I physically can’t do chest compressions (though I can coach any able-bodied person properly) but I can darned well use a mask with a one-way valve as if I’ve had years of practice. Years. You don’t have to have that (the training has shifted away from doing rescue breathing) but I feel that I do.

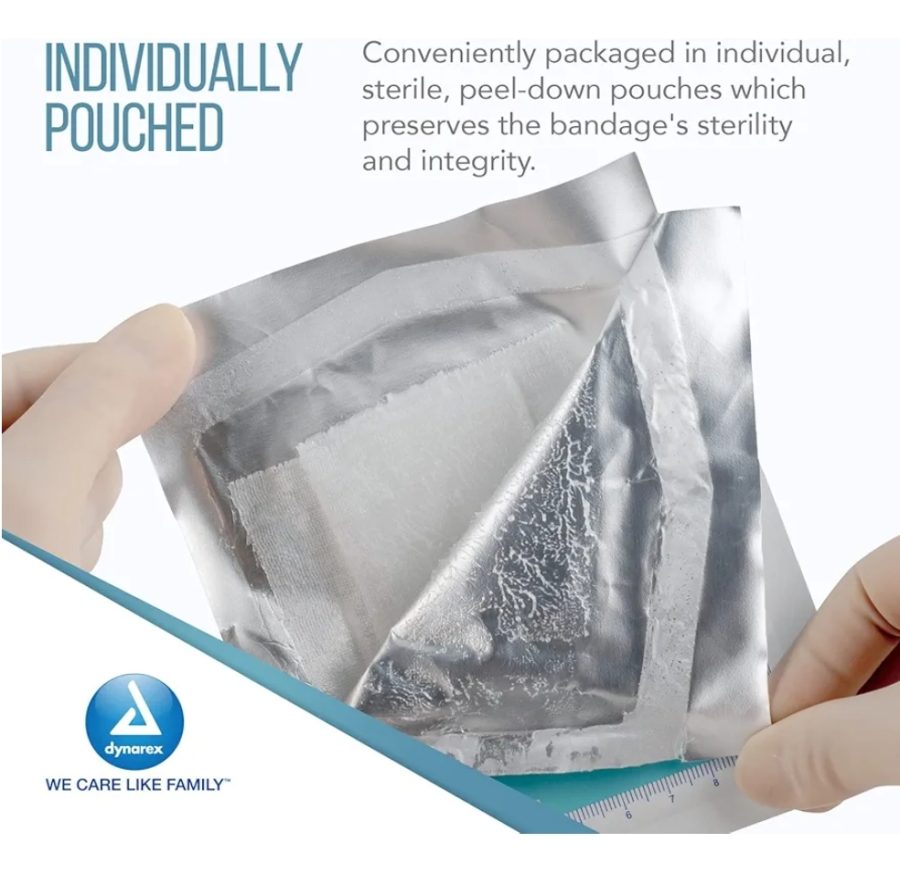
Pressure dressing? Kerlix. Sling? Kerlix. Wound cleaning? Kerlix makes a great sponge. Wound wrap? Kerlix. Piece of clean water-resistant paper to slap over a bubbling wound? Wrapping off a Kerlix.
So, plenty of Kerlix.

Road rash? Plenty of saline rinse (and a Kerlix) then a petroleum dressing to stabilize the damage until the ER can do a better job.

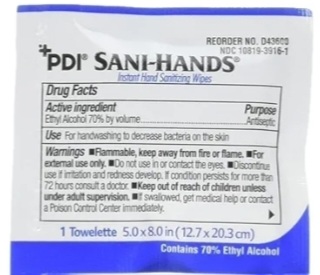
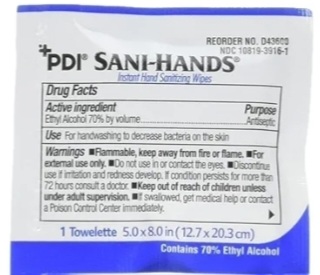
And possibly most essential: disinfectant cleansing towels, individually wrapped and big enough to grab. Those get used before if there’s time, during if the patient wants cleaning up, and definitely afterwards.
Because allergies & neurological reactivity, I stick with ethyl alcohol 70%.
Secure the mess. A gallon-sized zip bag or 2 for garbage and wrappings. Having a garbage bag is one of the things that separates rescuers from ego-trippers.
Oh, did I say that out loud? Sorry. I don’t want anyone not to stop & help… I just wish that, if they’re going to the effort of bringing gear, they could pick up a bit. Seeing blood and mess is not good for survivors & passers-by.
I got all these online for about $10 each, and also got a clear bag (with outside pockets) to put the kit in.

I’ll keep backstock at home.
What I don’t carry
Blood pressure readings, stethoscopes, and pulse oximetry are at-home and in-hospital concerns: we want to know if what we’re doing is working over time and refine our understanding of the body’sfunctional state.
In the field, the main issue is not whether the patient has rales or a murmur, but whether the lungs and heart are keeping them alive – a much simpler, larger-grained issue.
So, these tools might be nice to have, but for a noodle-noggin like me, they’re an added complication and a bunch of expensive equipment to lose at the scene.
In the field,
- You need to keep pulse and respirations going,
- the spine stable,
- make sure the inside stuff stays inside
- and in place,
- and (as much as possible) the outside stuff stays out – or at least doesn’t move much where it’s inside the person.
And that, ladies and gentlebeings, is Advanced First Aid and Basic Life Support in a nutshell. You’re welcome 😊 Now go get that training… please?